Procedure Steps
Simplifying Vasectomy Procedure Steps in Perth with Professional Care You Can Trust

What to Know About the Procedure for a Safe and Effective Vasectomy Experience
Many men worry about pain, risks, or long-term effects when considering a vasectomy. Concerns about discomfort, recovery, and possible complications can cause hesitation.
Understanding the procedure helps ease these worries. At Perth Vasectomy Centre, our experienced team uses patient-focused care and minimally invasive techniques to promote a safe and well-supported vasectomy experience.

Why Choose Perth Vasectomy Centre?
Experience
Dr. Essa Rasool has years of extensive experience performing vasectomies, offering confidence and professionalism throughout the entire process.
Reputation
Since 2017, patients have trusted us to provide reliable vasectomy services in a professional, welcoming, and patient-centred environment.
Comfort
The no-scalpel technique reduces discomfort, speeds up recovery time, and minimises risks compared to traditional vasectomy methods.
Convenience
We are centrally located in Ascot and Baldivis, with flexible appointment times, same-day bookings, and onsite parking for easy access.
Affordability
We offer transparent pricing with Medicare rebates and no hidden fees, making our vasectomy services accessible and budget-friendly.
Aftercare
Comprehensive follow-up care is provided to address any concerns so that our patients feel supported and comfortable after their procedure.
A Step-by-Step Guide to the Vasectomy Procedure

Apply Local Anaesthesia
Local anaesthesia is applied to numb the scrotal area, helping to enhance comfort throughout the vasectomy procedure.

Locate and Secure the Vas
The vas deferens is gently located and secured by the doctor to prepare for the next steps of the procedure.

Puncture Skin Layer
A small puncture is made in the scrotum to access the vas deferens in a controlled manner.
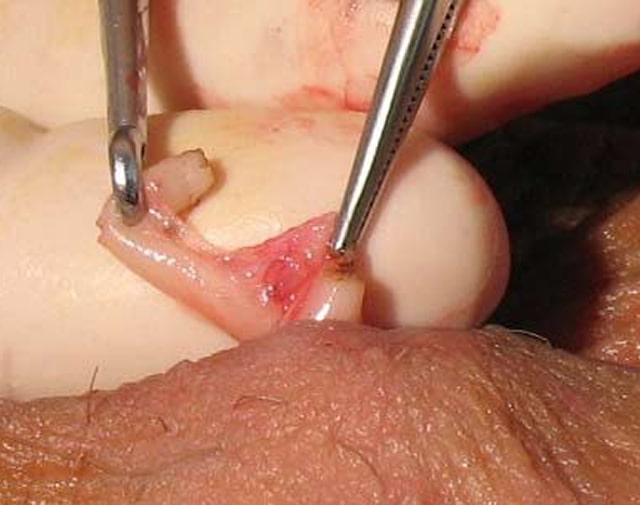
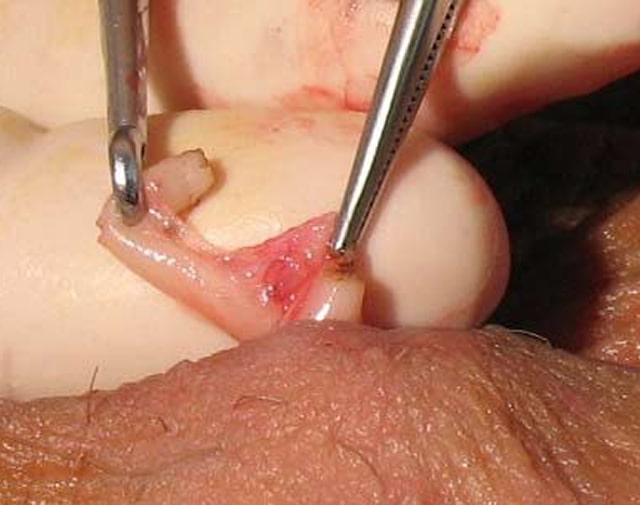
Divide and Interpose Fascia
The vas deferens is divided, and fascial interposition is used to help block the flow of sperm effectively.

Close Puncture Site
The small puncture site gradually closes without stitches, allowing for natural healing and reducing visible scarring.
Applying Local Anaesthesia for a Comfortable and Pain-Free Vasectomy Experience
The doctor applies local anaesthesia to the scrotum, numbing the area to help reduce discomfort during the vasectomy procedure.

Locating and Securing the Vas with Precision During the Vasectomy Procedure
The doctor carefully identifies and secures the vas deferens to stabilise it and allow accurate handling during the procedure.

Puncturing the Skin Layer Using Advanced Techniques for Minimal Discomfort and Healing
The doctor uses a sharp tool to create a tiny puncture in the scrotum, aiming to minimise discomfort and support natural healing without stitches.

Dividing and Interposing Fascia to Block Sperm Flow During the Vasectomy Procedure
This step involves placing a layer of tissue (fascia) between the cut ends of the vas deferens to help block sperm flow and reduce the likelihood of reconnection.
Closing the Puncture Site for a Safe and Seamless Vasectomy Completion
After the procedure, the puncture site gradually closes without stitches, supporting recovery and completing the vasectomy procedure with care.

Apply Local Anaesthesia

Applying Local Anaesthesia for a Comfortable and Pain-Free Vasectomy Experience
Locate and Secure the Vas

Locating and Securing the Vas with Precision During the Vasectomy Procedure
Puncture Skin Layer

Puncturing the Skin Layer Using Advanced Techniques for Minimal Discomfort and Healing
Divide and Interpose Fascia
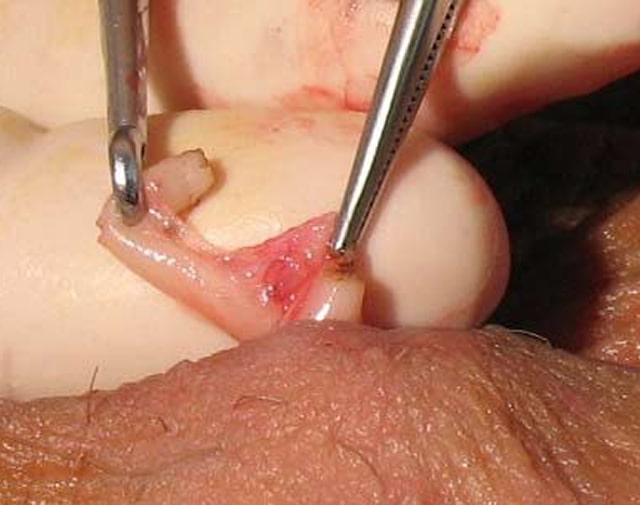
Dividing and Interposing Fascia to Block Sperm Flow During the Vasectomy Procedure
Close Puncture Site

Closing the Puncture Site for a Safe and Seamless Vasectomy Completion
DOCTOR'S PROFILE
Meet Dr. Essa Rasool

Dr. Essa Rasool
GP Obstetrician
Dr. Essa Rasool is a highly experienced medical professional with a career spanning decades. He spent 26 years at Rockingham General Hospital, delivering babies and providing exceptional care. Obtained a Medical Degree at Royal College of Surgeons in Dublin Ireland. He also earned a diploma from the Royal College of Obstetricians and Gynaecologists.
Now practising at the Ridge Medical Centres both in Ascot and Baldivis, Dr. Rasool provides care in areas like men’s health and vasectomy. A Fellow of the Royal Australian College of General Practitioners, he has been performing vasectomies since 1990 under local anaesthetic.
Dr. Essa Rasool
GP Obstetrician
Patient Resources Designed to Guide You Through Your Vasectomy Journey

Answers to Frequently Asked Questions About Vasectomy for Confident and Informed Decision-Making
Essential Preparation Tips for a Successful Vasectomy Experience

Vasectomy Aftercare Made Simple With Expert Guidance and Support

Frequently Asked Questions
Got a question we missed? Contact Us
What should I expect during a no-scalpel vasectomy consultation?
Before the procedure, you’ll have an initial appointment to discuss important details about the no-scalpel vasectomy process, providing clarity on what to expect.
- The doctor will explain the procedure, including how the vas deferens is accessed to help prevent sperm cells from mixing with semen.
- Your medical history will be reviewed to confirm suitability, especially if you have heart disease or other health problems.
- The possibility of infection, swelling, sperm leaking, or rare cases of post-vasectomy pain syndrome will be discussed.
- The surgical steps will be outlined, including local anaesthesia, using the single puncture technique, and sealing the vas deferens.
- Guidance on recovery will include advice on when to resume normal activities, such as exercise and sexual intercourse, while minimising discomfort.
- Post-procedure care instructions will highlight the importance of a semen analysis to confirm whether sperm are present in the semen.
- You’ll be advised to continue using other forms of contraception until the procedure is confirmed as effective in preventing pregnancy.
- Concerns about sex drive, sexual performance, the ability to ejaculate, and reversal surgery will be addressed, as the procedure typically does not affect these functions.
This consultation helps you understand the process, address any concerns, and decide if this is the right contraception option for you.
How is a no-scalpel vasectomy performed?
A no-scalpel vasectomy involves several careful steps to cut the vas deferens, the tubes in the testicles that carry sperm. Below is a step-by-step description of how vasectomy is performed:
- Preparation at the clinic or surgery centre:
The procedure is conducted in a clean and sterile environment. The scrotum is thoroughly cleaned to help reduce the risk of infection or other complications like bleeding. - Administering local anaesthetic:
A local anaesthetic is injected to numb the area around the scrotum’s skin. This helps minimise pain or discomfort during the procedure. - Locating the vas deferens:
The doctor palpates the scrotum to locate the two tubes that transport sperm from the testicles to the penis. - Creating a puncture:
Special instruments make a small puncture in the skin of the scrotum. The puncture is small enough to heal naturally without requiring stitches. - Accessing the vas deferens:
Each vas deferens is gently pulled through the puncture opening, one at a time, to avoid unnecessary trauma to the surrounding tissues. - Cutting and sealing the vas deferens:
Both vas deferens are cut, and the ends are tied or sealed. This procedure aims to prevent the sperm from entering the semen when the man ejaculates. At Perth Vasectomy Centre, fascial interposition is used, adding a layer of tissue between the cut ends to further support effectiveness. - Returning the vas deferens:
After the tubes are sealed or tied, they are returned to their original position inside the scrotum. The puncture is left to heal naturally. - Post-procedure care:
A dressing is applied to the puncture site. Patients are advised to use an ice pack to reduce swelling. They should also avoid strenuous activities such as heavy lifting for a few days.
This surgical procedure is considered an effective method of birth control for most men. It typically does not interfere with sexual performance, orgasm, or daily activities. Procedures to reverse the vasectomy may be available, but success rates vary.
What position are you in during a no-scalpel vasectomy?
What type of anaesthesia is used for a no-scalpel vasectomy?
Will I be able to see what's happening during the surgical procedure?
During the vasectomy procedure, the surgical area is draped to maintain sterility and privacy, which is a standard practice in surgical settings. You will not see the doctor accessing or cutting the vas deferens, which are the tubes that carry sperm in your semen from the testes.
This setup helps reduce the patient’s stress and limits exposure to blood or surgical instruments. The procedure allows the male patient to remain awake and helps maintain comfort under local anaesthesia.
How long do the actual no-scalpel vasectomy procedure steps in Perth take?
Although vasectomy surgery typically takes 20-30 minutes, several factors can influence its duration:
- Anatomy of the patient:
Variations in the position or size of the vas deferens may require additional time for the doctor to locate and access the tubes. - Previous surgeries or scarring:
A history of surgeries or injuries in the scrotum or surrounding areas can make the procedure more complex. - Patient’s comfort level:
If the patient feels anxious or uncomfortable during the procedure, additional time may be provided to help them stay at ease. - Local anaesthetic response:
The time it takes for the local anaesthetic to numb the area fully can vary, potentially adding to the overall duration. - Unexpected challenges:
In rare cases, complications such as difficulty accessing the spermatic cords or vas deferens may extend the procedure time. - Doctor’s technique and experience:
While an experienced doctor often completes the procedure quickly, individual approaches and methods can slightly vary the duration.
These factors are uncommon but can influence how long the vasectomy procedure steps in Perth take. The procedure is designed to be efficient while prioritising patient comfort and safety.
Do you get stitches in a no-scalpel vasectomy?
What is the recovery time for a non-surgical vasectomy?
The recovery time for a non-surgical vasectomy varies, but many patients recover within about one week. Around 80% of men return to normal activities within this period. The following steps may support recovery:
- Rest for 24 hours:
Avoid physical activity immediately after the procedure. - Wear tight underwear for 48 hours:
This supports the area and may help minimise discomfort. - Apply ice to the scrotum for 24–48 hours:
Ice can help reduce swelling and support healing. - Avoid cycling or strenuous activities for 7 days:
Minimising physical strain supports proper recovery. - Gradually resume normal activities:
Most patients feel ready to return to their routine within a week.
Following post-procedure care may aid recovery and reduce the risk of complications.
Will I feel any pain or discomfort during the no-scalpel vasectomy procedure?
What should I wear to the appointment for a no-scalpel vasectomy?
Choosing the proper clothing for your no-scalpel vasectomy appointment can help with comfort and post-procedure support. Here are detailed recommendations:
- Tight-fitting underwear or supportive briefs:
These help hold the scrotum in place after the procedure. Proper support may help minimise movement and reduce discomfort or swelling. Avoid boxers, as they do not provide enough support. - Loose, comfortable pants:
Opt for trousers or sweatpants with a relaxed fit. These make it easier to move around post-procedure without adding pressure to the area. - Avoid restrictive belts or tight waistbands:
These could press against the surgical area, potentially causing discomfort. - Clean and easy-to-wash clothing:
The procedure is sterile, but wearing clean clothes helps maintain hygiene.
These clothing choices may aid recovery. Tight underwear provides compression, which can help reduce movement and support swelling management.